This executive summary highlights the key findings and recommendations from the California Golden Fleece® Award briefing, COVID in California: How Government Regulations Created Critical Healthcare Shortages — Permanent Patient-Centered Reforms Needed .
OVERVIEW
On January 19, 2020, the first documented US case of the novel coronavirus (COVID-19) appeared in the state of Washington. Easily transmittable, the virus found its way to California shortly thereafter in February—the same month that the first nontravel-related (“community spread”) case in the United States was confirmed in Solano County, California. On March 19, eight days after the World Health Organization officially declared the COVID-19 outbreak a pandemic, California governor Gavin Newsom (D) signed Executive Order N-33-20, a statewide shelter-in-place order resulting in months of quarantine for tens of millions of people.
In the initial months of the COVID-19 response, California, like many other states, was woefully unprepared and lacked the degree of flexibility required to adequately respond to the pandemic. The labor market for medical personnel was constrained, medical equipment suffered from undersupply, hospitals were under stress, testing was inadequate, and potential treatments suffered from a suboptimal economic environment—despite many past warnings. A 2005 report published by the US Homeland Security Council, for example, warned of the potential threat of a widespread viral pandemic, stating that, “States and communities should have credible pandemic preparedness plans to respond to an outbreak within their jurisdictions. The private sector should play an integral role in preparedness before a pandemic begins and should be part of the national response.”
Officials at all levels of government failed to heed this call to action. Perhaps even worse, regulatory barriers prevented rapid and efficient private-sector responses, fueling the crisis and harming healthcare consumers. In the end, the public policy response played a high-stakes game of catchup as government-imposed regulatory straitjackets created breaking points in California’s healthcare system.
For enacting or enforcing regulations that created critical healthcare shortages and that prevented a fast, efficient response to COVID-19 by public and private entities, the Independent Institute awards its eleventh California Golden Fleece® Award to a host of federal and state officials and regulatory agencies, including the California legislature; Governor Gavin Newsom; past California governors; the US Centers for Disease Control and Prevention (CDC); the US Food and Drug Administration (FDA); US Centers for Medicare and Medicaid Services; US Customs and Border Protection (CBP); labor unions, professional associations, and boards representing medical personnel; and those representing the nation’s flawed intellectual property laws.
Political Failure in the Healthcare Industry
COVID-19 exposed the ways in which regulations are used in California to benefit narrow interest groups at the expense of consumers at large. In the healthcare sector, these interest groups represent occupations (e.g., physicians, nurses, pharmacists), providers (e.g., hospitals, clinics, urgent care centers, pharmacies), and suppliers (e.g., medical device manufacturers, drug developers). Each interest group typically has its own lobbying entity, such as the California Hospital Association.
By supporting government regulations that raise artificial barriers to entry, these interest groups are able to increase their incomes, profits, and political influence. They have also learned that the surest means of blocking competition is to “capture” the regulatory machinery of governments and use it to create protected cartels that benefit privileged groups (their own members) while harming unorganized consumers. In addition to the resultant enforcement and administration costs, innovative lifesaving drugs and devices are delayed and competition among providers is short-circuited, thus increasing prices and reducing patient access to higher-quality care.
Equipment and Labor Shortages
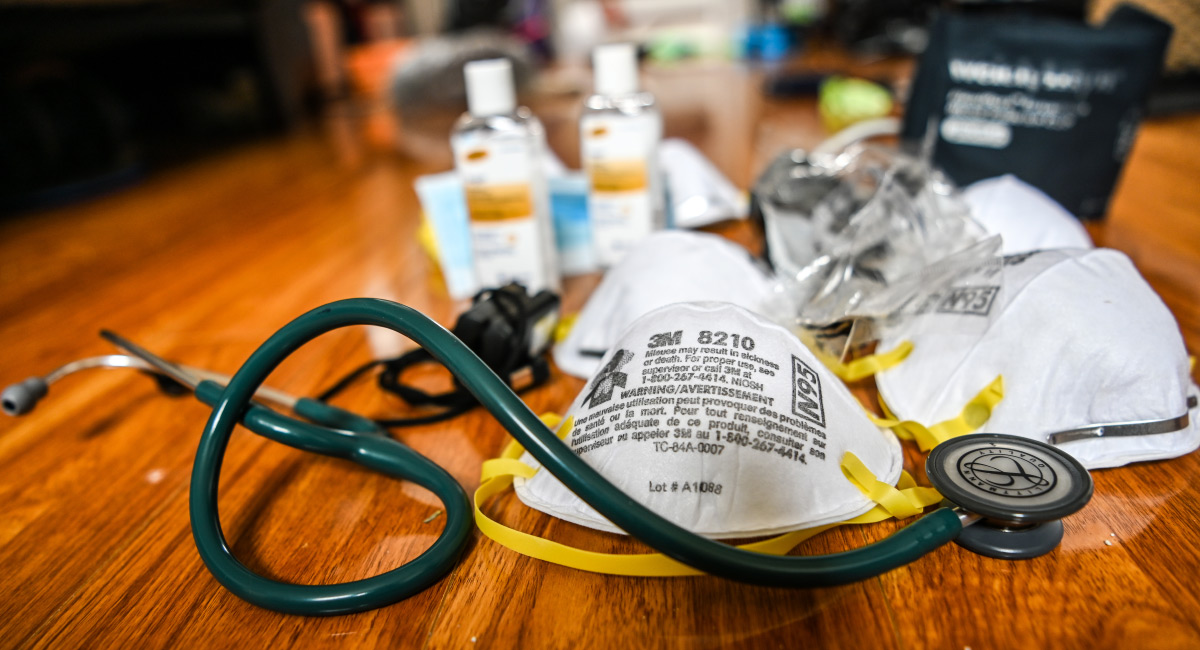
Despite multiple warnings years before the COVID-19 outbreak, governments did not stockpile critical supplies adequately and maintained regulatory barriers that prevented fast and efficient market responses by private-sector entrepreneurs wanting to alleviate emerging shortages.
Governments also protected incumbent manufacturers of personal protective equipment (PPE), ventilators, and other medical equipment from domestic and foreign competition, using public safety as the justification. For example, the state of California erected barriers to the rapid importation of foreign-made products and the rapid manufacture by domestic producers. That political strategy proved to be destructive during the COVID-19 pandemic. While regulations benefited companies such as 3M over the years, they were deadly obstacles to obtaining needed supplies quickly after COVID struck. Public safety was sacrificed to benefit politically connected interest groups. And although officials eventually adopted emergency liberalizations, by then much harm had already occurred to both patients and healthcare workers.
Personnel scarcity. Regardless of the adequacy of medical supplies, if enough healthcare workers are not available, patient care will suffer. And it’s important to keep in mind that California suffered from severe shortages of healthcare workers before the outbreak. The pandemic only exacerbated these shortages, which became worse from early 2020 through early 2021 although they were largely avoidable if not for the staggering number of government rules that artificially restrict the supply of qualified healthcare personnel and limit their optimal allocation.
The stated justification for such strict government controls has been ensuring patient safety, but the controls go beyond what is needed and do not allow market signals to determine where additional workers are required and with what skill sets. Once in place, the regulations prevent rapid adjustment to changing circumstances. Healthcare workers who are qualified and available to work are excluded from the market; thus, the supply of healthcare workers is artificially restricted, which is especially harmful during a crisis.
For example, the California Board of Registered Nursing (CBRN), which operates much like a medieval guild, limits the number of students who can attend nursing school. Any shortage of nurses, therefore, is never a case of individuals electing not to enter the field—nor is it the case that not enough people met the high standards that the field demands. To the contrary, according to the CBRN’s own reporting, more than twenty-one thousand qualified nursing students were denied enrollment during 2016−2017, or 60 percent of all qualified applicants.
Facing a statewide nursing shortage during a pandemic, the CBRN continued to keep enrollment caps in place, a morally reprehensible act. These professional cartels hampered training and prevented employment levels from adjusting to market demands based on price signals.
Eventually liberalizations were adopted: Qualified healthcare workers from out of state were allowed to work in California (albeit with approval from the government after filing paperwork). Retired workers were welcomed back. Scope-of-practice restrictions and staffing ratios were relaxed, giving supervisors more flexibility. Licensing requirements were also eased to allow faster hiring of healthcare personnel and more allocative flexibility.
These were sweeping improvements that should be continued in perpetuity in order to help healthcare patients and medical personnel—pandemic or no pandemic. If it is the right thing to do now, it is the right thing to do in the future.
Botched COVID 19 Testing
Early in the COVID-19 outbreak, it became clear that communities needed rapid, inexpensive, frequent testing. Yet procuring tests was a disaster from the start. The CDC botched the initial rollout and covered up its mistakes, while at the same time the FDA prevented private alternatives from reaching the market. Only after opening up the testing market to private innovators and more laboratories was progress made; yet the goal of rapid and frequent at-home nonprescription testing has not been achieved after one year—an unmitigated disaster that has cost lives and devastated the economy due to government-imposed lockdowns.
Eventually, test manufacturers—in partnership with a number of agencies, including the National Cancer Institute—were allowed to send in samples voluntarily to verify testing accuracy. But the policy was short lived and commercial test developers were required to request emergency use authorizations with their validation data, a step backward from previous FDA protocol. During this time, the United States fell behind in its per-capita testing levels—with California becoming one of the nation’s most visible examples of poor testing rollouts.
Vaccines, Treatments, and Therapeutic Antiviral Drug Development
The most important success story to emerge from the COVID-19 pandemic has been the fast development of several (hopefully widely effective) vaccines. It is important to note that this resulted from unleashing the innovative potential of nongovernmental research entities—most of them private pharmaceutical companies—while at the same time minimizing government interference in the creative process. In fact, Pfizer explicitly rejected US government research grants in order to maintain its independence and “keep Pfizer out of politics.”
Nevertheless, for a variety of reasons, including a confusing tiered prioritization system and a clunky software platform called PrepMod, California has struggled to get its allotted vaccines into people’s arms. In fact, during the first four weeks of vaccine distribution, only Alabama, Georgia, and Virginia performed worse than California in vaccinating its population. The state vaccinated only 2,468 people per 100,000 compared to the national average of 3,300.
Despite the stumbling vaccine rollout, however, this recent liberalized approach to vaccine development has the potential to accelerate new drug development significantly in the future.
Patient-Centered Recommendations
During the first months of the COVID-19 outbreak, government healthcare regulators tried to do business as usual, but it quickly became apparent that regulations, designed to benefit incumbents, were causing a worsening crisis in care. Americans deserve a more responsive healthcare system that is able to respond to new circumstances quickly and nimbly; that provides convenient, high-quality care at affordable prices; and that encourages rapid innovation to fight emerging threats and offer lifesaving breakthroughs. The following reforms would help patients significantly:
1. Allow private companies in the United States and abroad to supply the equipment demanded by the healthcare sector. Healthcare providers should be able to source needed products from private manufacturers in the United States or around the world without licenses or permits as long as each manufacturer certifies that its products are FDA compliant or compliant with the standards of a private governing body. The default should be “permissionless innovation and competition,” with any damages stemming from problematic products to be remedied in the civil courts through tort proceedings.
2. Abolish scope-of-practice rules and staffing ratios. Research demonstrates that adverse health outcomes have not occurred when states relaxed their scope-of-practice rules. Eliminating such rules would help restore the flexibility that healthcare facilities need to function efficiently. For example, a study in Medical Care Research and Review found no differences in health status between patient groups assigned to a nurse practitioner versus a primary care physician two years after treatment. Another study published in 2018 in the Journal of Health Economics found that health outcomes were comparatively better after scope-of-practice laws were eased.
3. Reduce practice barriers for nursing and all other healthcare occupations. Government occupational licensure of the healthcare industry is not needed. In fact, evidence that licensing results in better health outcomes is spurious. Additionally, a white paper prepared by the Department of the Treasury, Council of Economic Advisers, and Department of Labor during the Obama Administration found that despite the increased costs due to licensing laws, consumers are not receiving better health services. It is simply impermissible that, facing a nursing shortage amidst a pandemic, the CBRN would maintain its program admissions caps.
4. Permit interstate and international competition in healthcare occupations by allowing a freer flow of talent. Consumers benefit from the increased choices that result from rigorous competition among providers. California should therefore open its market to qualified healthcare workers in other states. Too many foreign-born physicians in the United States drive taxis, work at car washes, or manage supermarkets instead of saving lives only because cartel regulations and visa restrictions protect native US residents from competing with foreign-born doctors.
5. Free up testing by allowing private companies to provide tests, testing sites, and testing laboratories without government approval. Both the state of California and the US government proved early on to be incapable of providing fast and reliable mass testing for COVID-19. As public outrage increased, government officials relaxed rules to encourage private-sector participation and innovation. As with medical supplies, the standard should be permissionless innovation, holding companies accountable for fraud or damages through criminal or civil court proceedings. The same approach should become the norm for all testing, not just for COVID-19.
6. Permanently allow telemedicine across state lines. State licensing laws have stifled the development of telemedicine, because such laws restrict the practice to only those who are licensed in the state. However, it is difficult for many people to visit a clinic or hospital for care, especially older persons and people with disabilities. Telemedicine is therefore an invaluable development that lowers the opportunity costs for people seeking medical evaluations and consultations.
During the interme of the pandemic, a number of governments waived these licensing laws that targeted telemedicine. In the state of California specifically, the original Proclamation of a State of Emergency and Executive Order N-43-20 lifted limits on telemedicine, while a Medicaid waiver allowed for the reimbursement of payable claims by out-of-state telehealth providers. At the federal level, a HHS waiver relaxed regulations as well.
7. Speed the development and deployment of new vaccines and therapeutic drugs. A number of reforms could be continued or adopted that would speed up the development of new vaccines and therapeutic drugs. Ten years, on average, to develop a new vaccine is nonoptimal. A number of reforms are worthy of further consideration:
- The federal government should continue and expand the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) program to expedite clinical trials and accelerate the review of trial data.
- The mandate of the FDA should be changed to require evaluating only the safety of a proposed new drug, not its efficacy. As a result, initial R&D costs would be reduced, and a strong case could then be made for shortening the duration of pharmaceutical patents. (Any FDA delays in approving a given drug could be tacked onto the duration of the patent equal to the actual delay.) If this is prevented, complex arrays of property rights, or “patent thickets,” can form, reducing the application of new ideas and making it more difficult to commercialize new products.
- Drugs approved in select foreign countries should be allowed on the US market, with appropriate disclosures. This reciprocity would permit drugs to reach consumers quicker in the United States, bypassing FDA regulatory bottlenecks. Reciprocity should apply to medical devices and PPE as well.
- Patent applications should be published immediately. Prior to 1995, applicants could abuse the patent system and hold secret patent rights that might “surface” during legal disputes, earning them the moniker of “submarine patents.” Now patents generally get published eighteen months after their priority date. This reform is a noted improvement; however, innovation could benefit from further transparency.
- Operation Warp Speed should be wound down, but its “prize” feature should be adopted widely in the United States and around the world. Under a prize model, governments, private nonprofits, and other entities could offer lump-sum grants—$5 billion, for example—to a company or partnership that develops a drug for curing an identified disease. This prize model reduces government interference in research and development while freeing entrepreneurs to innovate.
- A variation of the prize model advanced by Nobel laureate economist George Stigler includes a stipulation that prevents the prize “winner” from patenting the new knowledge as a condition of receiving the grant. Such a stipulation would replace patent protection with a lucrative prize and allow the world’s scientific community to learn from and utilize the new knowledge immediately.
In addition to these reforms, a number of other COVID-19–related regulatory changes that have already been implemented on a temporary basis should be continued permanently or even expanded. These include, but are not limited to, the emergency liberations found in Table 1.
These changes should be adopted permanently regardless of when the next healthcare crisis strikes. Such reforms are the moral response because they will improve the lives of people today and of future generations by facilitating better access to affordable, high-quality care and more lifesaving breakthroughs—a win for all patients regardless of the existence of a pandemic.
| Table 1. EMERGENCY LIBERALIZATIONS THAT BENEFITTED CALIFORNIANS | |
| Personal Protective Equipment and Medical Equipment | FDA authorized, in multiple EUAs, the use of unapproved medical products and unapproved uses of approved products if the company certifies the product is FDA compliant. Products include PPE, medical devices, diagnostic tests, ventilators, and more. |
| FDA allowed unlicensed companies to manufacture PPE and medical equipment. | |
| FDA fast-tracked the importation of PPE and medical devices subject to an EUA. These new rules were implemented by CBP. | |
| Trump Administration activated the Defense Production Act to compel production of medical equipment, to prevent the exportation of PPE, and to mobilize the military for COVID assistance. | |
| Healthcare Personnel | State scope-of-practice rules eased. |
| State licensing, certification, training, and staffing ratios relaxed for healthcare occupations and facilities. | |
| State rules streamlined to more quickly hire inactive/retired healthcare professionals and qualified out-of-state medical personnel. | |
| Some state training rules for nursing students waived, allowing the students to graduate early and be hired sooner. | |
| COVID-19 Diagnostic Testing | FDA reversed course, allowing commercial manufacturers to sell tests to laboratories without an FDA EUA (this was later reversed). |
| Test manufacturers could voluntarily send samples to government and academic labs to verify the accuracy of the manufacturer’s test (later reversed). | |
| FDA transferred to states oversight responsibility for lab-developed tests. | |
| Newsom Administration turned to the private sector and signed mass-testing contracts with OptumServe, PerkinElmer, and Verily. | |
| FDA issued EUAs for at-home, self-administered test kits developed by Lucira and Abbott (prescription required) and by Ellume (OTC). | |
| Vaccines and Therapeutic Drugs | Predevelopment and postdevelopment government funding of promising vaccines and therapeutics through Operation Warp Speed. |
| Channeled payments through a private contractor to expedite the process (OTAs). | |
| Expedited clinical trials and the review of trial data through the ACTIV program. | |
| FDA issued EUAs for monoclonal antibody therapies and COVID-19 vaccines. | |
| Source: The table was compiled by the authors using material in this report: Lawrence J. McQuillan, Jonathan Hofer, and Douglas E. Koehler, COVID in California: How Government Regulations Created Critical Healthcare Shortages — Permanent Patient-Centered Reforms Needed (Independent Institute, April 2021). | |